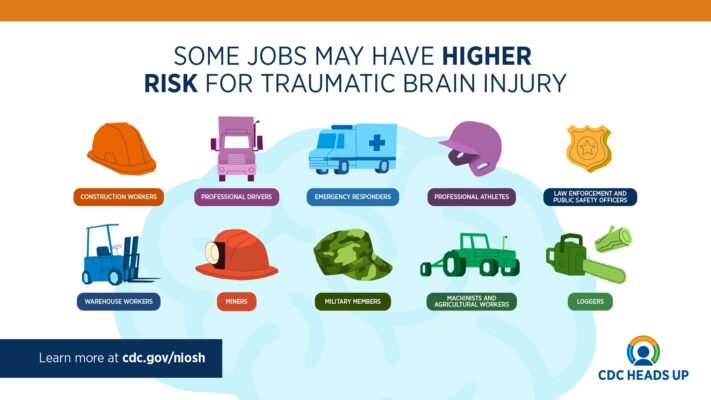
Image of some jobs that may have higher risk for TBI
Understanding TBIs: A Comprehensive Guide to Traumatic Brain Injuries On The Job
Traumatic brain injuries (TBI), including concussions, can occur in any type of workplace. However, research shows that some workers may be at increased risk for TBI. 12Some examples include those who work in Construction, General and Specialized Freight Trucking, and Services to Building and Dwellings industries, as well as U.S. Service members.12
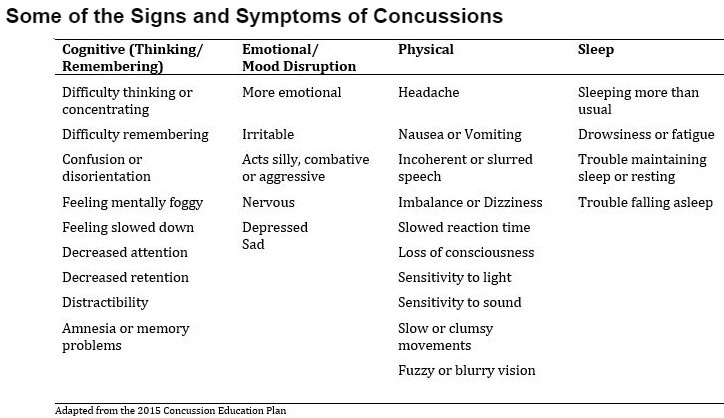
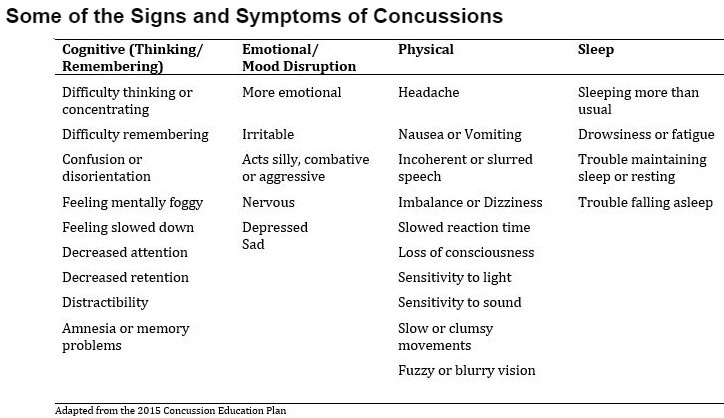
Signs and Symptoms of a TBI: What to Look Out For
TBI symptoms may include problems with thinking, concentration, reaction time, and emotions, as well as feeling more tired than usual. Some symptoms may affect a person’s ability to do their normal work activities. Symptoms may last for months or even years,3 and for some, may involve co-occurring health conditions, such as post-traumatic stress disorder (PTSD) and depression.45
What to do? TBI Recovery is a complex process that requires comprehensive care and support.
Healthcare providers have treatments available to help support recovery from a TBI, including symptoms related to mental and physical health.6 They can also provide instructions on when a worker can safely return to work and list any needed supports or accommodations.
Employers can connect an employee to an Employee Assistance Program and offer support services, including mental health support, when the person returns to work to help speed their recovery.67
Employees can learn more about federal protection and leave programs that may be available following an TBI or other injury.
Returning to work after a TBI
Returning to work after a TBI is different for each person and depends on many factors, including:
- Severity of the injury and symptoms
- Tasks employees are required to perform as part of their job
- Types of symptoms people are experiencing
Some people with a TBI can return to work within a couple of days of their injury and may only need short-term support or accommodations during their recovery, like rest breaks during the day or earplugs to limit sensitivity to noise. Others may need weeks, months, or longer before returning to work. Some people may not be able to return to work (or the same type of employment) due to long-term disability or persistent symptoms.
Workers may need more time off after a TBI if their job requires:
- Working from heights, including climbing a roof or ladder, or the risk of falling
- Exposure to explosions, blasts, or projectiles
- Intense physical activity, such as running and heavy lifting
- Attention or concentration
- Driving
- Operating machinery or heavy equipment
- High-stress or safety risks, such as work with hazardous materials
These activities may make an employee’s symptoms worse or increase their chance for another brain injury during recovery.
A healthcare provider may recommend employers make changes to an employee’s tasks or schedule during their recovery.
Examples of accommodations for employee with a TBI include:
- Rest breaks, shortened work schedule, or a later start time
- Time to take short walks or other similar light physical activity
- Temporary transfer to a position with tasks that don’t worsen symptoms
- Access to sunglasses, earplugs, or headphones if bothered by light or noise
- Reduced driving or physical activity
- Extended time to complete tasks
- Reduced screen time, such as on computers and tablets
- Limited or no use of machinery or heavy equipment
- Access to assistive technology to help perform tasks, like screen reading and magnification software
The jobs of public safety officers (such as law enforcement, firefighters, and emergency medical care providers) can include tasks that involve intense physical activity, operating vehicles, and high stress situations.
Employers of public safety officers may consider providing alternate tasks for public safety officers recovering from a TBI when possible.
Resources
There are many organizations helping people with a TBI and their family during recovery. See the Where to Get Help webpage for more information on organizations that can provide support for persons living with a TBI and their families.
CDC’s National Institute for Occupational Safety and Health develops partnerships, conducts research, and implements intervention strategies focused on improving workplace safety.
More information on TBI and other injuries among service members, Veterans, and public safety officers are available from CDC and other federal agencies. Examples include:
- The Report to Congress on Traumatic Brain Injury in the United States: Understanding the Public Health Problem among Current and Former Military Personnel [PDF – 130 pages], developed by CDC, the National Institutes of Health, the Department of Defense, and the Department of Veterans Affairs, includes an overview of TBI among service members and Veterans. It also includes several considerations to address this important public health problem.
- Data on TBI among service members and Veterans can be found on the Department of Veterans Affairs website. Visit the Military Health System’s Traumatic Brain Injury Center of Excellence website for more information and support for service members, Veterans, and families and caregivers.
Lt. Col. Tim Maxwell’s Story
Read more about Lt. Col. Tim Maxwell’s recovery from a severe TBI sustained during military deployment. Lt. Col. Tim Maxwell’s Story (cdc.gov)
See References below
When to Seek Immediate Medical Attention for TBI
Danger Signs in Adults
In rare cases, a person with a concussion may form a dangerous blood clot that crowds the brain against the skull. Contact your health care professional or emergency department right away if you experience these danger signs after a bump, blow, or jolt to your head or body:
- Headache that gets worse and does not go away.
- Weakness, numbness or decreased coordination.
- Repeated vomiting or nausea.
- Slurred speech.
The people checking on you should take you to an emergency department right away if you:
- Look very drowsy or cannot wake up.
- Have one pupil (the black part in the middle of the eye) larger than the other.
- Have convulsions or seizures.
- Cannot recognize people or places.
- Are getting more and more confused, restless, or agitated.
- Have unusual behavior.
- Lose consciousness.
Danger Signs in Children
Take your child to the emergency department right away if they received a bump, blow, or jolt to the head or body, and:
- Have any of the danger signs for adults listed above.
- Will not stop crying and are inconsolable.
- Will not nurse or eat.
References:
- Konda S, Al-Tarawneh IS, Reichard AA, Tiesman HM, Wurzelbacher SJ, Pinkerton LE, Meyers AR, Hendricks SA, Tseng CY, Lampl MP, Robins DC. Workers’ compensation claims for traumatic brain injuries among private employers-Ohio, 2001-2011. Am J Ind Med. 2020 Feb;63(2):156-169. doi: 10.1002/ajim.23073.
- Department of Defense. Numbers for Traumatic Brain Injury Worldwide. Available at: https://health.mil/Military-Health-Topics/Centers-of-Excellence/Traumatic-Brain-Injury-Center-of-Excellence/DOD-TBI-Worldwide-Numbers.
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Report to Congress on traumatic brain injury in the United States: Epidemiology and rehabilitation. Atlanta (GA): Centers for Disease Control and Prevention; 2015.
- Mac Donald CL, Johnson AM, Wierzechowski L, et al. Outcome trends after US military concussive traumatic brain injury. J Neurotrauma. 2017;34(14):2206-2219. doi:10.1089/neu.2016.4434.
- Smith NIJ, Gilmour S, Prescott-Mayling L, Hogarth L, Corrigan JD, Williams WH. A pilot study of brain injury in police officers: a source of mental health problems? J Psychiatr Ment Health Nurs. 2021;28(1):43-55. doi:10.1111/jpm.12676.
- LeGoff DB, Wright R, Lazarovic J, Kofeldt M, Peters A. Improving outcomes for work-related concussions: a mental health screening and brief therapy model. JOEM. 2021;63(10):e701-e714. doi:10.1097/jom.0000000000002350.
- Gaudette É, Seabury SA, Temkin N, et al. Employment and economic outcomes of participants with mild traumatic brain injury in the TRACK-TBI Study. JAMA Netw Open. 2022;5(6):e2219444-e2219444. doi:10.1001/jamanetworkopen.2022.19444.

