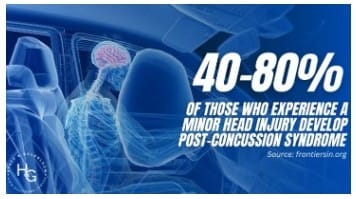
It is crucial to seek medical attention immediately after any head injury for a thorough evaluation and monitoring, even if symptoms seem minor at first.
Early detection allows for prompt treatment to prevent further injury and a head start on rehabilitation.
Read More
Recognizing a traumatic brain injury isn’t always straightforward—many individuals may be unaware of their own symptoms or dismiss them entirely. IT IS NOT ALWAYS THEIR FAULT!
That’s why family, friends, and loved ones play a critical role in identifying signs and encouraging proper care.
READ MORE – When TBI Signs Aren’t Obvious
Here are some guidelines for recognizing a possible TBI when the person is oblivious to their own symptoms…
Your Loved Ones Can Help You.
They can….
- Gently ask questions – “You seem a little off today. Have you noticed anything different?”
- Observe patterns – if symptoms persist or worsen, document them for medical professionals.
- Encourage medical evaluation – even if they resist, suggest seeing a doctor “just to be safe.”
- Provide reassurance – avoid making them feel defensive; instead, express concern with care.
- Watch for worsening symptoms – if they seem to be declining, seek medical help immediately.

Since TBI symptoms can be subtle, having trusted people around to notice changes can make all the difference in early intervention and recovery.
If you or someone you love has experienced a fall, accident, or head injury and is noticing changes—however small—it’s worth exploring further.
The TBIQ questionnaire can help determine if symptoms align with a traumatic brain injury and provide clarity on the next steps.
tbiq
 IDENTIFY TBI
IDENTIFY TBI

 DR DIAGNOSIS /Rx
DR DIAGNOSIS /Rx

50% of those people don’t even realize it!
The injury can actually prevent the Brain from recognizing TBI!
OR, the Brain tries to put the missing pieces together, but has the wrong info!
Symptoms can appear to be unrelated, and many are afraid to tell anyone!
Many suffer in silence ~ not telling family, friends, doctor, lawyer, employer – sometimes for YEARS!
You can quickly skim the list of symptoms to identify a concussion/TBI with TBIQuikList.
THEN, you can complete the TBIQ (51 symptoms + you can write about the traumatic event) to provide to your Doctor.
Your Doctor can quickly skim the TBIQ. YOU DO NOT NEED TO TALK which might be stressful for you.
Your Doctor can quickly view ALL of your symptoms, and won’t need to cut you off!
This is much more efficient, and you’ll have more time to discuss your treatment & Healing Journey!
Even a MILD TBI is a PERMANENT BRAIN INJURY.
Read More
Click Links Below
TBI Questionnaire (English) TBI Questionnaire (Espanol) Letter to TBI Survivor (English)
Carta a un Sobreviviente de TBI (Espanol)
Letter to TBI Survivor’s Healthcare Provider (Give this to Dr with completed TBI Q)
Print these QUESTIONS to ask Your Physician so you can take them with you.
![]()
- Use the TBIQuikList to identify symptoms in under a minute
- Download the TBIQuestionnaire to take to your doctor
- Visit TBI-U/Self-Rehab for articles, research, and healing tools
- Explore resources for military, first responders, educators, parents, students, seniors, survivors of violence, high-risk professions, sports
- Browse the BEST APPS & PRODUCTS and SHOP pages for curated support tools

This website was created by me, Karen Renee Gomez…ALONE… A Survivor of over 12 TBIs and a TBI advocate helping TBI clients during my 40-year legal career as a Paralegal ~ many of the clients didn’t even know they had a brain injury, or they were afraid to tell anyone, until they talked to me!
I founded TBI-ID.com in January 2025. Over the past year, I’ve built more than 100 pages of FREE Resources to help individuals and families IDENTIFY & RECOGNIZE TBI symptoms. RESPOND (seek medical attention), then start the Healing Journey to RECOVER from traumatic brain injury (TBI).
I DID IT! MANY TIMES! YOU CAN DO IT, TOO!!!
If you’d like to support this work,
Donations can be made directly through this site.
If this website has helped you or someone you love, please consider supporting my ongoing work to keep it FREE and accessible for EVERYONE.
THANK YOU FOR YOUR GENEROUS SUPPORT!
DID YOU KNOW. . .Many people don’t realize they have a TBI – until years later, when symptoms become overwhelming.
Flint Rehab “Recovery is possible even decades after a TBI. We’ve seen patients 24 years post-injury regain function through consistent rehab and neuroplasticity-based exercises.” (Flint Rehab article)
TBI-ID.com was created to help people identify silent, potentially life-threatening TBIs – so they can start their Healing Journey.
Your support helps keep this platform free, updated, and accessible for everyone who may be walking through symptoms they don’t yet understand.

Many people don’t realize they have a TBI – until years later, when symptoms become overwhelming.
LEFT UNTREATED. . .
A traumatic brain injury (TBI) can lead to serious long-term conditions such as:
-
Chronic headaches and migraines
-
Seizure disorders (including post-traumatic epilepsy)
-
Cognitive decline and early-onset dementia
-
Depression, anxiety, and mood instability
-
Hormonal imbalances due to pituitary dysfunction
-
Sensory processing disorders (vision, hearing, touch)
-
Motor coordination issues and balance problems
-
Impulse control and behavioral changes
-
Increased risk of neurodegenerative diseases like Alzheimer’s and Parkinson’s
These effects may not appear right away – but they can quietly erode quality of life, relationships, and independence over time.
That’s why early Awareness (recognition), Screening (TBIQ confirmation), and Self-Advocacy (Self-Rehab Therapies ~ available on our website!) are essential, and the sooner you start, the better!!!
FREE SELF-REHAB THERAPIES (50+)
so you can begin your HEALING JOURNEY TODAY!
(Includes Art Therapy, Aquatic Therapy, Breathing Exercises, Biofeedback, Color Therapy, Hypnotherapy, Memory Games, Music Therapy, Neuropathy, Occupational Therapy, Pet Therapy, Reading, Reflexology, Sound Therapy, Strength Training, & More!)
Sample FREE e-Newsletter from Flint Rehab 7/8/25
This Week in Recovery ~ July 8, 2025 ~ Brain Injury
Gaining Weight After a Brain Injury? Here’s Why—and What to Do. Weight gain after TBI is common and frustrating—but it’s manageable. Learn what causes it and how to stay on track. Read the article
Saying the “Wrong Thing” After Brain Injury? Here’s What’s Going On. Disinhibition can cause emotional outbursts or impulsive comments—but it’s not your fault. Learn how to manage this common post-TBI symptom. Read the article

Flint Rehab’s newsletter provides free rehabilitation resources including expert tips and insights, exercise guides, and more – forward this email/link to invite a friend.
Your Free Recovery Resources
Each Self-Rehab Therapy on our website includes a link (or will) to Flint Rehab’s published research, offering credible support for its therapeutic benefits.
Flint Rehab empowers TBI survivors to take recovery into their own hands, offering home-friendly exercises and therapeutic tools that can be used anytime, anywhere. Their trusted resources—including hundreds of expert-written articles and interactive rehab devices—are featured throughout TBIQ to help you take action and see results.
Researchers at Flint Rehab confirmed that just 10-15 minutes a day…can reawaken the brain’s ability to heal itself (“Neuroplasticity”) and strengthen the neural connections that support memory, focus, mood, and daily function. It will also help build new ones, support cognitive recovery, and improve overall brain resilience – especially when combined with aerobic activity that boosts oxygen and nutrient delivery to the brain. (Click Here for Flint Rehab’s article about 30 Brain exercises!)
Want even more guidance? Explore Flint’s free rehab eBooks or watch home-based brain exercise videos (YouTube) to get started today.
Why the TBI Questionnaire Exists
After multiple TBIs over five decades and witnessing countless survivors (40 years as a PI paralegal) struggle to be heard, I knew something had to change. Too often, doctors rush through appointments, dismiss and ignore symptoms, or unknowingly trigger trauma by forcing survivors to verbally recount their injury- especially in cases of military-related TBIs and PTSD, and violent assaults.
The TBI Questionnaire (TBIQ) was created as a silent interlude, a way for patients to document symptoms at home and hand the completed form to their doctor – eliminating the stress of verbal explanations while ensuring nothing critical is overlooked, saving a lot of precious time. This creates more quality time to spend with your physician for the Plan.
This tool is designed to: ✅ Improve efficiency – Doctors can quickly review symptoms in an organized format. ✅ Reduce emotional burden – Patients can provide full details without verbal triggers. ✅ Ensure comprehensive care –Medical providers get a clear picture of long-term effects and daily struggles.
For many Survivors – especially those in the military community – this simple step can make appointments more productive, respectful, and trauma-sensitive. No more feeling ignored, rushed, or unheard – just real, structured support for recovery.
——————————————
This TBI Questionnaire* has been designed to provide a standardized, efficient, and comprehensive way for TBI survivors to document their symptoms when they are at home, and they can take as much time as they need. It aims to enhance communication between patients and healthcare providers, reduce stress for patients, and ensure consistency in care.
TBI Questionnaire (English) TBI Questionnaire (Espanol) Letter to TBI Survivor (English) Carta a un Sobreviviente de TBI (Espanol) Letter to TBI Survivor’s Healthcare Provider (goes with a copy of your completed TBI Q)
* TBI Questionnaire is a structured, self-report tool that helps survivors document their symptoms, ensuring they have a clear, standardized way to communicate their experiences with healthcare providers. These references reinforce the credibility of this approach and show that it is grounded in established screening methods. (References below)
__
These sample Questionnaires will only give you an idea of the type(s) of Questionnaire(s) your healthcare provider has or might have.
There are a few short 1-page versions, as well as a 7-page version for people who have been suffering for 3 months or longer (which is included FYI, but meant for Providers).
There are also TBI Guides, information from the Department of Defense, and a 211-page document on the Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans.
1 STANFORD concussion-questionnaire-simple 1 page.pdf (Stanford Healthcare)
2.The Rivermead Post Concussion Symptoms Questionnaire* (1 page)
3. Acute Concussion Evaluation (Heads Up Clinicians) – 1 page Questionnaire (w/ 1 pg of instructions, etc.
4. Traumatic Brain Injury: A Guide for Patients (13 pages) (This guide was provided by the CogSMART program of the VA San Diego Healthcare System. The material presented is based on published scientific research and clinical studies and was adapted from a variety of sources)
5. SINCE THIS IS FOR PROVIDERS, IT IS INCLUDED “FOR YOUR INFORMATION ONLY“ – Microsoft Word – Materials for referring providers – concussions past 3 months.docx (Stanford Healthcare [Concussion & Brain Performance] – 7 pages)
DEPT OF DEFENSE: VETERANS
6. Assessment and Management of Dizziness and Visual Disturbances Following Concussion/Mild Traumatic Brain Injury: Guidance for the Primary Care Manager (Dept of Defense)
7. Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans (211 pages)
Additional Resources:
The Ohio State University TBI Identification Method (OSU TBI-ID), Brain Injury Screening Questionnaire (BISQ), and Neurobehavioral Symptom Inventory (NSI) all align with the symptoms and focus areas covered in TBI Questionnaire.
- OSU TBI-ID focuses on lifetime history of TBI, identifying patterns of injury that may contribute to cognitive, emotional, and behavioral challenges.
- BISQ is designed to screen for symptoms related to attention, memory, mood, impulsivity, and physical effects of TBI.
- NSI tracks post-concussive symptoms like dizziness, headaches, fatigue, memory issues, and emotional regulation difficulties.
- CDC research highlights the importance of structured self-report screening tools in diverse settings to identify individuals with undiagnosed or untreated TBI.
Ohio State University TBI Identification Method: OSU TBD ID I Ohio State Brain Injury Prevention & Rehabilitation
Brain Injury Research Center Screening Tools | Icahn School of Medicine
Health.mil – Neurobehavioral Symptom Inventory form


 Treatment Plan
Treatment Plan